Health
Survey Indicates Potential Doubling of Weight-Loss Drug Coverage by U.S. Employers in 2024
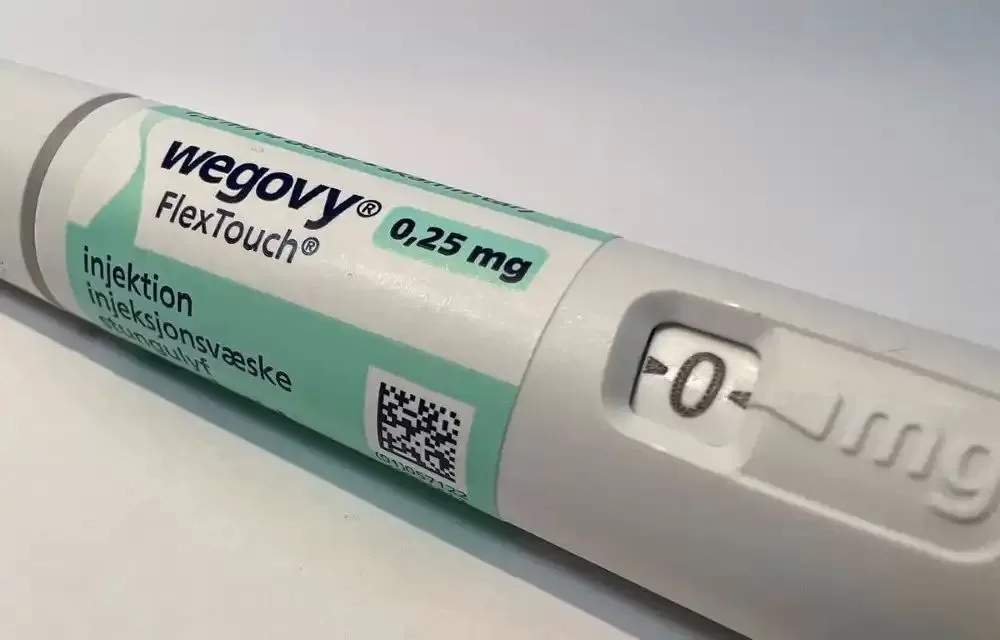
In a recent survey conducted by Accolade, a leading provider of employer healthcare programs, in collaboration with research firm Savanta, it was revealed that the number of U.S. employers considering coverage for obesity medications, including Novo Nordisk’s Wegovy from the class of GLP-1 drugs, is poised to nearly double in the upcoming year. Currently, 25% of surveyed employers offer coverage for GLP-1 drugs, whereas a substantial 43% are considering including them in their healthcare programs in 2024.
GLP-1s, or glucagon-like peptide 1 agonists, are primarily employed in the treatment of type 2 diabetes and for facilitating weight loss.
Accolade’s Associate Chief Medical Officer, James Wantuck, recommends a physician-led approach for the 43% of employers intending to introduce GLP-1 medication coverage next year. This approach will help guide the appropriate prescription of GLP-1 medications and integrate them effectively into a comprehensive health management plan.
Remarkably, almost all companies currently providing coverage for GLP-1 drugs have expressed their intention to continue doing so in the upcoming year.
However, employers offering coverage for weight-loss drugs are expected to face a surge in their healthcare costs due to the escalating popularity of Wegovy. Sales of Novo Nordisk’s Wegovy, along with its diabetes drug Ozempic, both containing the active ingredient semaglutide, have experienced significant growth in the past year. Additionally, Ozempic has seen ‘off label’ use for weight loss.
Furthermore, the demand for Eli Lilly’s Mounjaro, another GLP-1 diabetes drug anticipated to receive approval for weight loss treatment in the U.S. this year, has witnessed a remarkable increase.
Benefits consultant Aon has projected that a 1% increase out of the anticipated 8.5% rise in employer healthcare costs for the next year can be attributed to employee adoption of weight-loss drugs.
This transformation in employer-sponsored healthcare coverage reflects a growing recognition of the importance of addressing obesity and associated health concerns in the workforce. As 2024 approaches, the landscape of employer-provided healthcare programs is poised to evolve significantly, potentially providing more comprehensive support for those seeking weight management solutions.