Health
Microrobots in Neurosurgery: Small Size, Big Promise
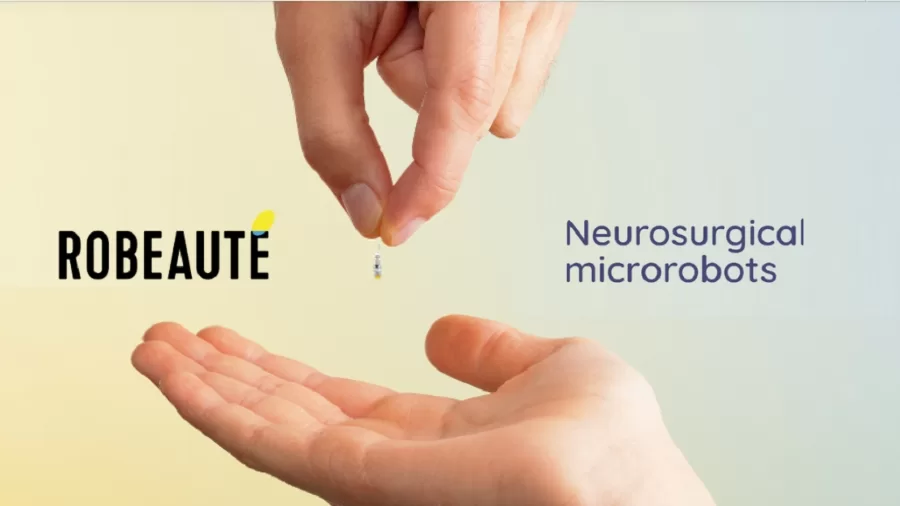
- French startup Robeauté unveils 3mm microrobots designed for delicate brain procedures.
- These devices promise to reduce surgical trauma and open new possibilities for hard-to-reach brain areas.
The first time I saw the prototype, I could barely see it. About the size of a rice grain, this device from French startup Robeauté could redefine brain surgery. Sitting on a stainless tray, the tiny tool didn’t look like much. Until they turned it on.
It moved.
It curved.
It responded to signals in real time, mimicking the trajectory it would take inside a patient’s brain.
This wasn’t just another lab demo. This was the first step in a shift that might change how neurosurgeons reach tumours, sample tissue, and deliver treatment in some of the brain’s most sensitive areas.
After the presentation, I spoke with Dr Emilie Chevalier, one of the lead roboticists on the project. She described the goal simply: “We want to go where no tool has safely gone before.”
What Is It, and Why Now?
The Robeauté microrobot is a 3mm surgical device designed to operate where conventional instruments can’t. Traditional tools follow fixed, linear paths. That’s limiting in brain surgery, where avoiding even a millimetre of healthy tissue can be critical.
This microrobot is different. It can move through curved trajectories. It slips through a burr hole roughly the size of a sesame seed, navigates the brain’s terrain, and delivers therapy or samples without disturbing healthy structures.
Unlike rigid scopes or instruments, the robot is flexible and responsive. Onboard sensors provide feedback in real time. Surgeons watch the feed and steer as needed.
The scale isn’t the only breakthrough. It’s what this scale allows: less bleeding, fewer complications, and the possibility to treat previously inoperable conditions.
From Bench to Brain: What It Can Do
Brain tumour biopsies are high-risk, especially in deep or critical regions. In many cases, patients aren’t candidates for surgery at all.
The microrobot may offer a way in. It can collect tissue without the collateral damage of traditional methods.
The device is also being tested for:
- Targeted drug delivery to localised tumour sites
- Placement of electrodes for movement disorders
- Ablation of micro-lesions using energy pulses
During my visit, the team showed simulation footage of the robot administering treatment to a simulated tumour target. Precision was within 0.1mm.
That kind of accuracy matters when every bit of tissue counts.
The Numbers Behind the Project
As of 2024, the global surgical robotics market is valued at over £12 billion, with neurosurgery accounting for an estimated 14% of this total. The rise in minimally invasive procedures has contributed to this segment growing at nearly 13% year over year.
The NHS performs roughly 30,000 neurosurgical procedures annually, with more than 5,000 involving tumour biopsies or resections. Even a 10% adoption of microrobotic assistance could translate into hundreds of procedures with potentially better outcomes and shorter inpatient stays.
This isn’t a university spinout with a single grant. Robeauté has secured €27 million—about £23 million—from a mix of public and private sources.
That includes French venture firms, EU research funds, and medical foundations. The funds are aimed at scaling development, completing pre-clinical work, and preparing for human trials.
Trials are scheduled to begin in 2026, starting with low-risk patients undergoing exploratory biopsies.
The team expects to pursue CE marking by 2028 and seek UK MHRA clearance in parallel.
What It Could Mean for the NHS
The NHS has been a global reference point for adopting new technologies. If Robeauté succeeds, the benefits could be significant:
- Faster surgeries, reducing OR occupancy times
- Fewer post-op complications, reducing patient re-admission
- Lower costs per procedure through shorter hospital stays
It’s not just about improving outcomes. It’s about system-wide impact. With neurosurgical cases placing pressure on limited theatre availability, a technology that speeds things up without compromising safety would be welcomed.
I spoke to a senior neurosurgical fellow at King’s College London. She told me bluntly, “If this tech delivers even half of what they promise, we’ll need to train every registrar on it within five years.”
From Paris to London: When Could It Arrive?
Robeauté plans to partner with hospitals in Paris, Brussels, and London during its initial trials.
The UK has been named as a potential site for a late-phase trial arm. Hospitals such as UCLH and the Queen Square Neuroscience Centre are early contenders for inclusion.
This matters for local adoption. If UK neurosurgeons are part of the testing process, uptake is more likely post-approval.
It’s a fast-moving timeline. Within 18 to 24 months, we could see early patient outcomes that determine the fate of the technology.
Training and Adoption
Technology alone doesn’t change surgery. Training does. Robeauté is already developing simulation modules for its device, allowing surgical trainees to practise with VR-linked consoles.
The modules replicate brain pathways using patient-derived imaging, letting trainees ‘drive’ the robot in virtual space.
A training program built into the tech rollout is a smart move. It also positions Robeauté as a long-term player, not just a prototype firm.
If approved, the company expects to offer certification courses to neurosurgical trainees in France, the UK, and Germany by 2027.
What To Watch As Trials Begin
As a journalist covering health innovation, here’s what I’m tracking:
- Early patient safety data and complication rates
- Comparative performance vs traditional tools
- Willingness of NHS trusts to invest in post-trials
- Integration into surgical education programs
If the tech proves reliable, expect major names in medical devices to explore partnerships or acquisitions.
This could also set a precedent for microrobotics in other fields. Think ENT, cardiac, and even gastrointestinal surgery.
Beyond Surgery: A Platform for Other Therapies?
There’s already talk of using the platform to deliver gene therapies directly into brain lesions. Others are discussing its use in real-time monitoring of tissue environments, such as measuring pH or oxygenation at the site.
A 3mm robot isn’t limited to what it does today. As payload options expand, so will their applications.
We may be at the beginning of a broader category of precision intervention devices.
Closing Thoughts
Sometimes medical innovation feels like it’s miles away from the bedside. But this isn’t one of those stories.
This is a 3mm leap that might make all the difference in operating theatres, patient outcomes, and health system economics.
If it works, you’ll hear about it in major trials, medical journals, and—eventually—from patients who avoided a craniotomy thanks to a tool no larger than a grain of rice.